Electronic Prior Authorization Automation: A Key to Achieving 10X Productivity & Velocity
5 months ago
Prior authorization is hard to manage, there is no doubt about it.
Because it is,
- Time-consuming for healthcare provider
- Costlier for healthcare practices
- Tedious for the payers
Almost 94% of physicians in the USA said that prior authorization delays care for 90% of their patients.
The primary reason behind it is the manual workflows that are surrounded by tedious phone calls.
But you can change that and make this hectic process less frustrating and more productive.
How?
With electronic prior authorization software!
It has got potential to bring peace of mind into the lives of providers, payers, and patients.
And you’ll know how in the next 3 minutes!
What is Electronic Prior Authorization?
For some medical and prescription care plans, healthcare providers need to take approval from the payers before performing it.
This process is called prior authorization.
However, this entire process is mostly performed manually for treatment and medication plans.
It includes data entry, documentation, phone calls, emails, and fax.
But an electronic prior authorization automation eliminates it easily and securely.
It automates the entire manual process!
From submitting requests to check eligibility and documentation to getting approvals.
Thus, the prior authorization process gets faster for everyone involved in it.
Who Can Automate Prior Authorization?
Electronic prior authorization automation is not just limited to providers.
It also assists pharmacy businesses and healthcare payers in streamlining all their workflows associated with it.
If you are one of them, you can implement automated electronic prior authorization software into your practices.
How Does Electronic Prior Authorization Software Equipped with RPA Tech Work?
Let’s understand it with a simple example.
We assume that you are a healthcare professional and want to perform a medication-related prior authorization process using the software.
So in that case, you will have to follow the streamlined workflow mentioned below.
(Note: The software is integrated with the EHR.)
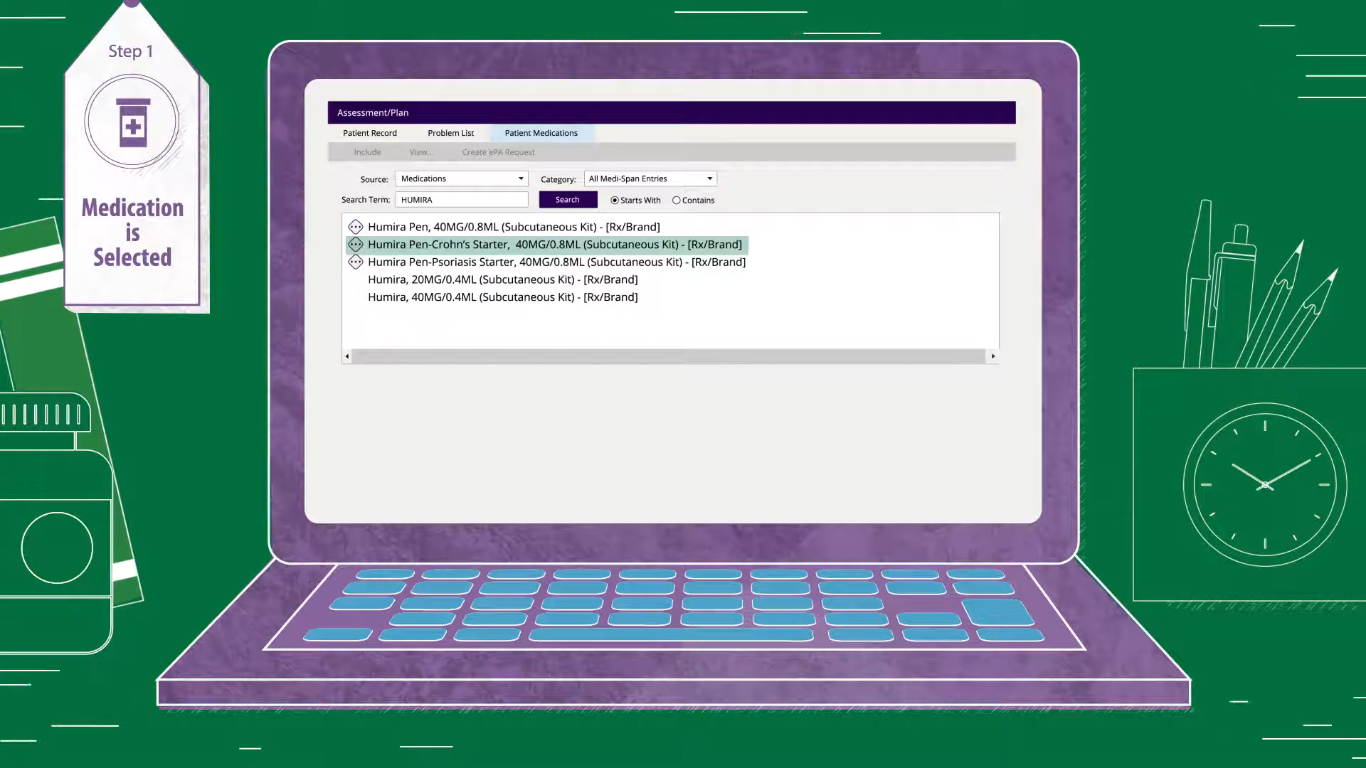
Step 1: Select the medication
As the electronic prior authorization software is already integrated with the EHR, you just need to select the prescription plan for the patient.
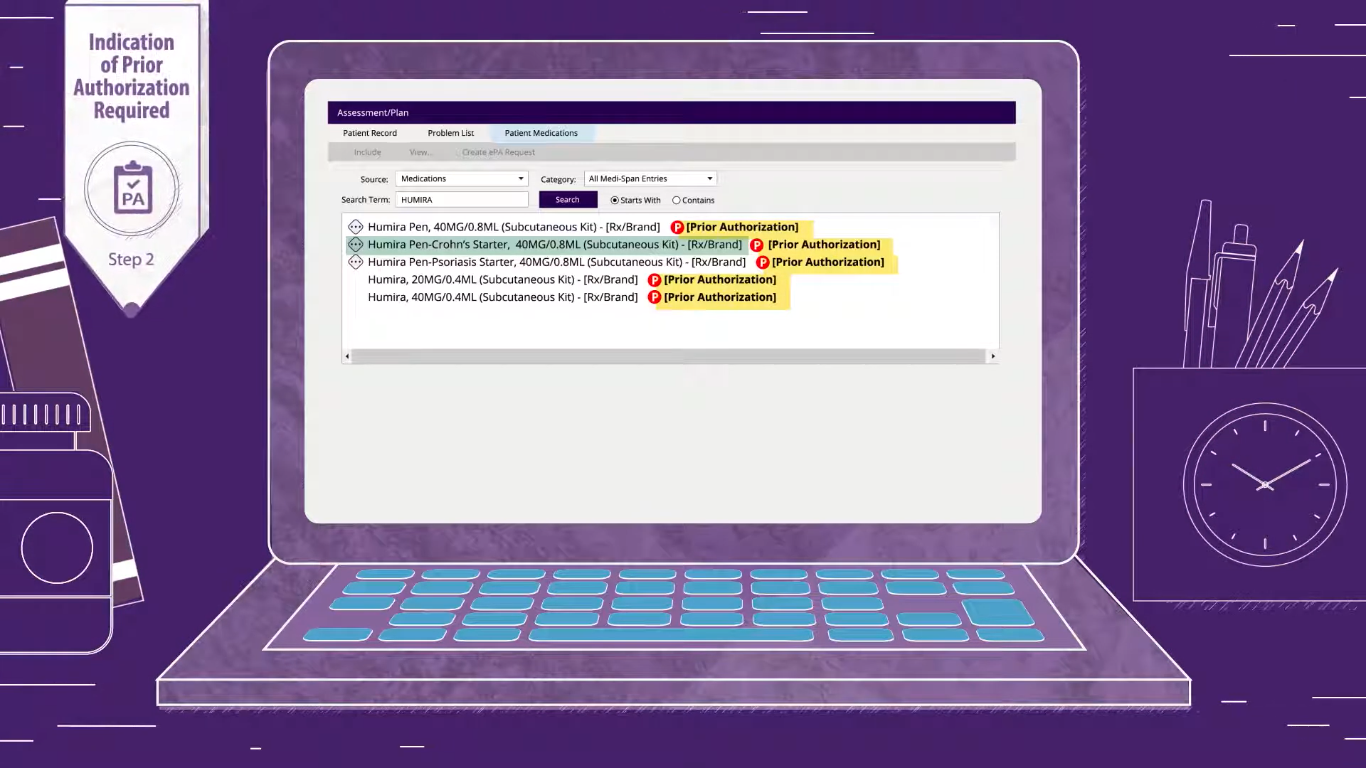
Step 2: Check the prior authorization requirement
The software will automatically show you the prior authorization requirements for the selected medication.
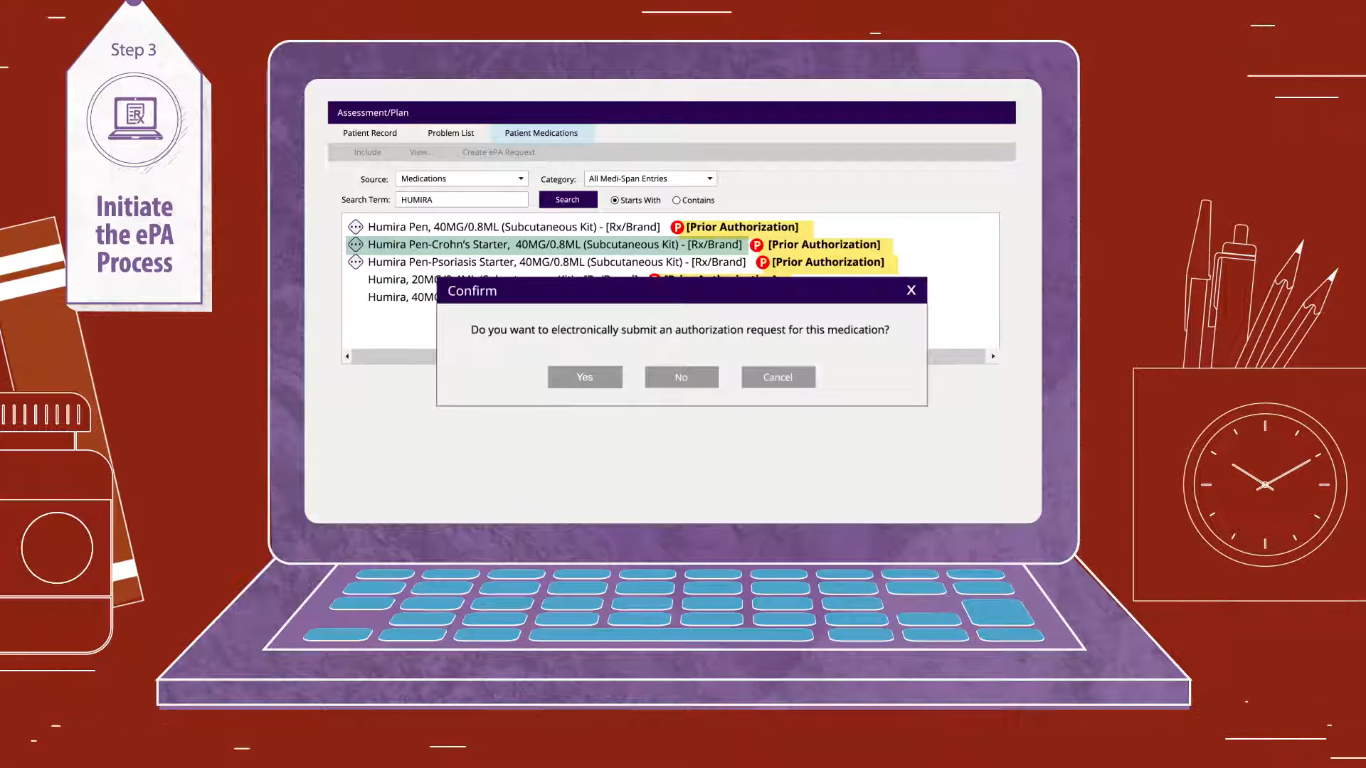
Step 3: Submit the electronic prior authorization request
If the medication plan you selected requires prior authorization, you’ll need to perform the entire process before sending the prescription note to the pharmacy store.
And for that, the first step is to submit the request.
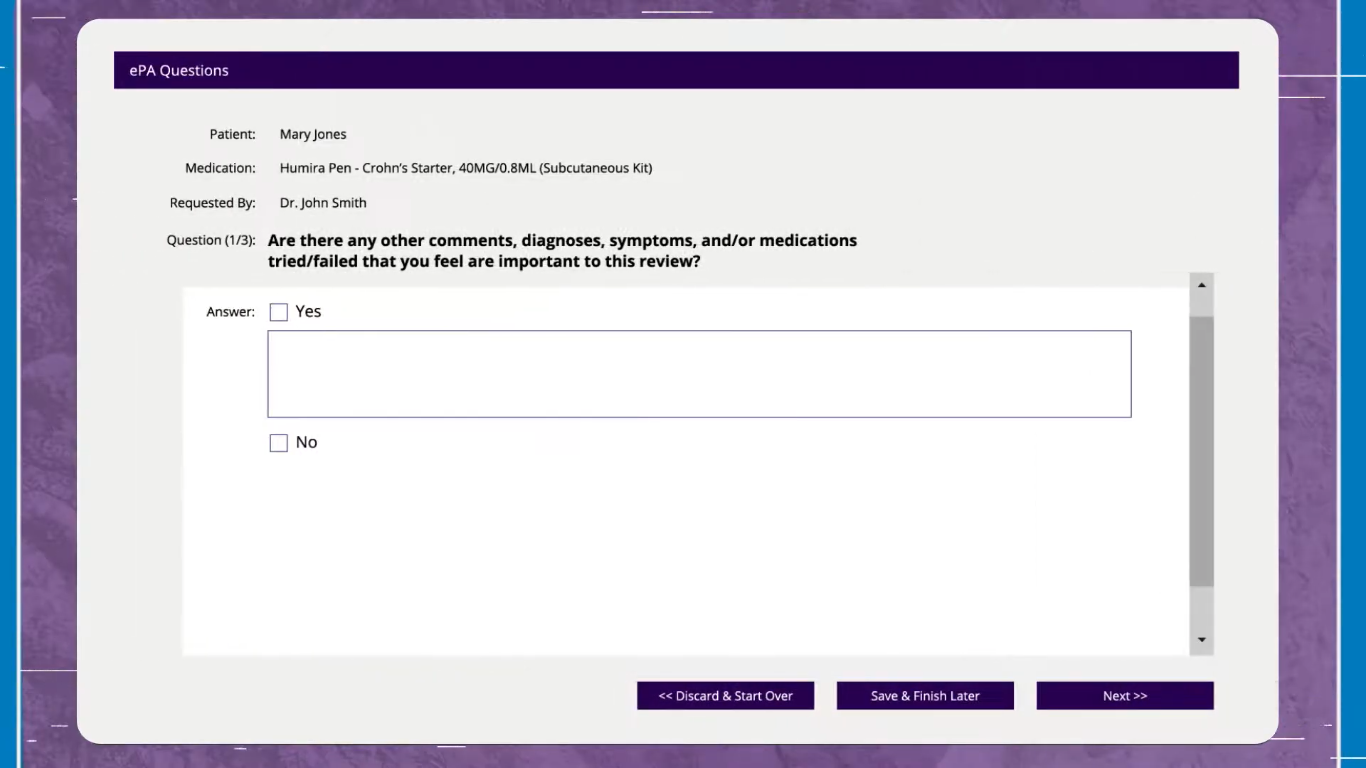
Step 4: Answer questions
Once you submit the electronic prior authorization, the software will ask you a few questions.
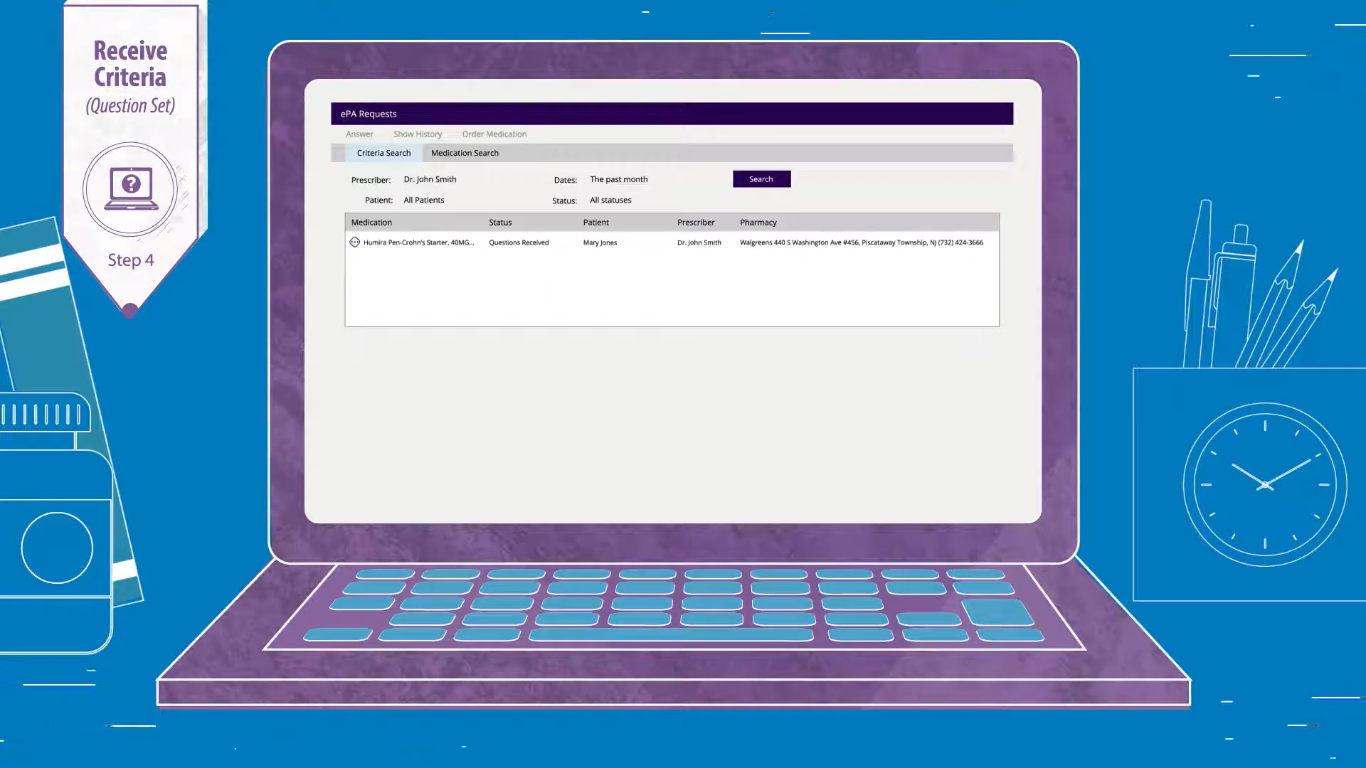
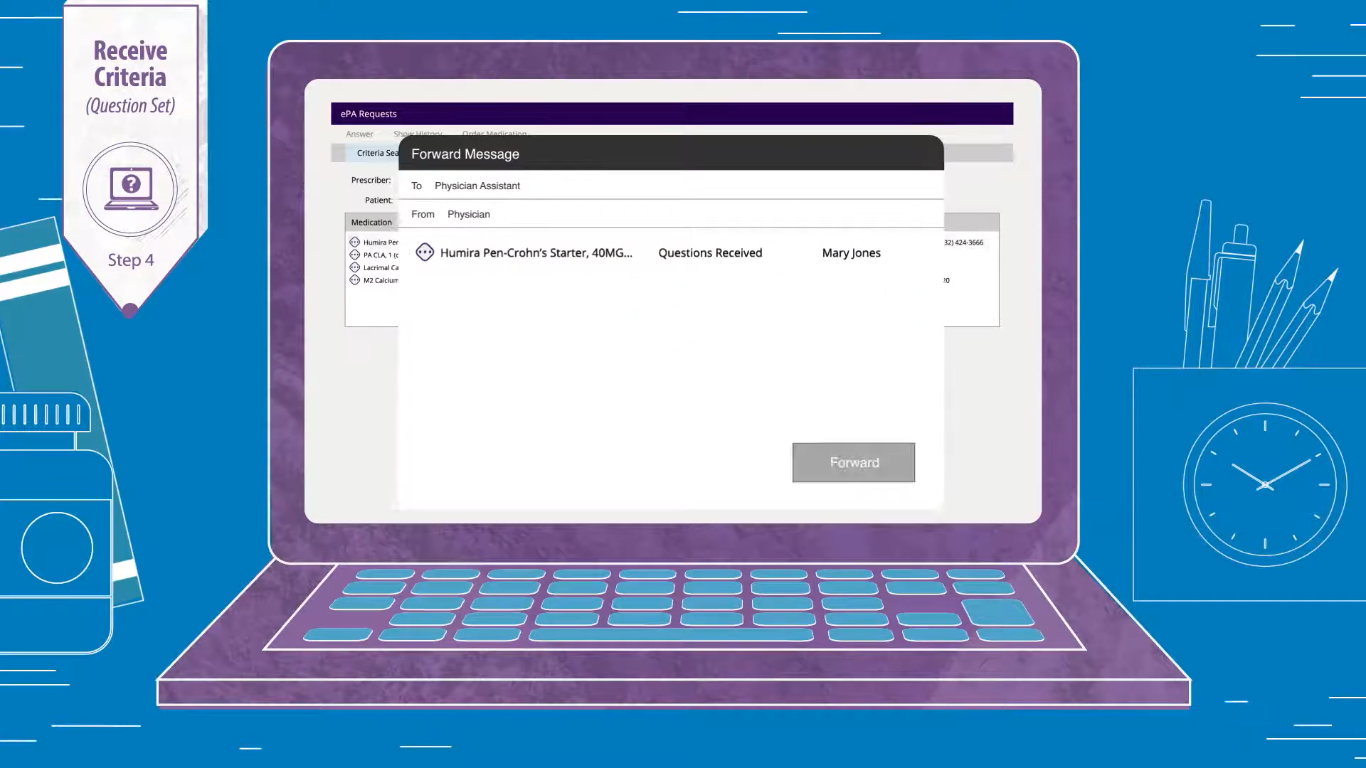
And these questions directly sync into the EHR.
This feature helps the other physicians and staff members to complete the process on your behalf.
These questions may be related to the selected medication plan or pharmacy benefits – in various forms.
For example,
1. True False
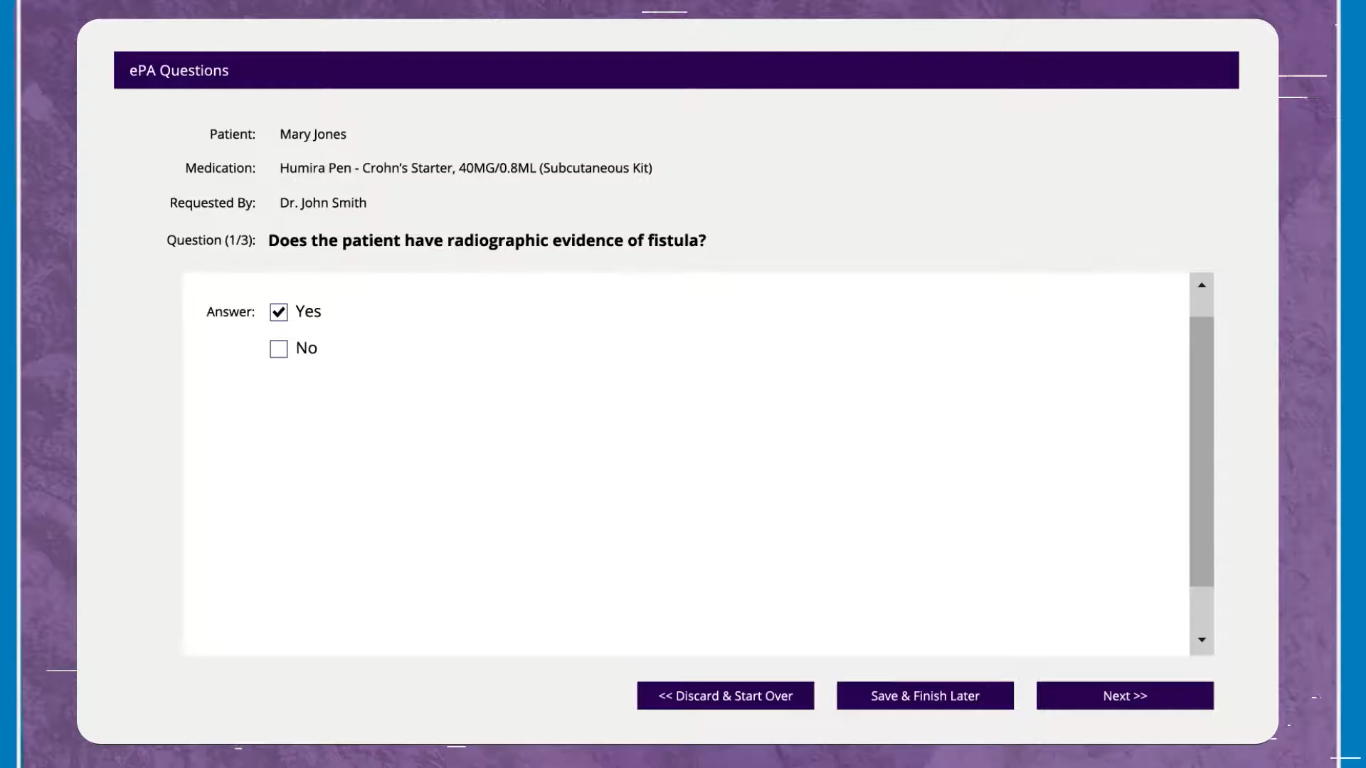
2. Multiple choice
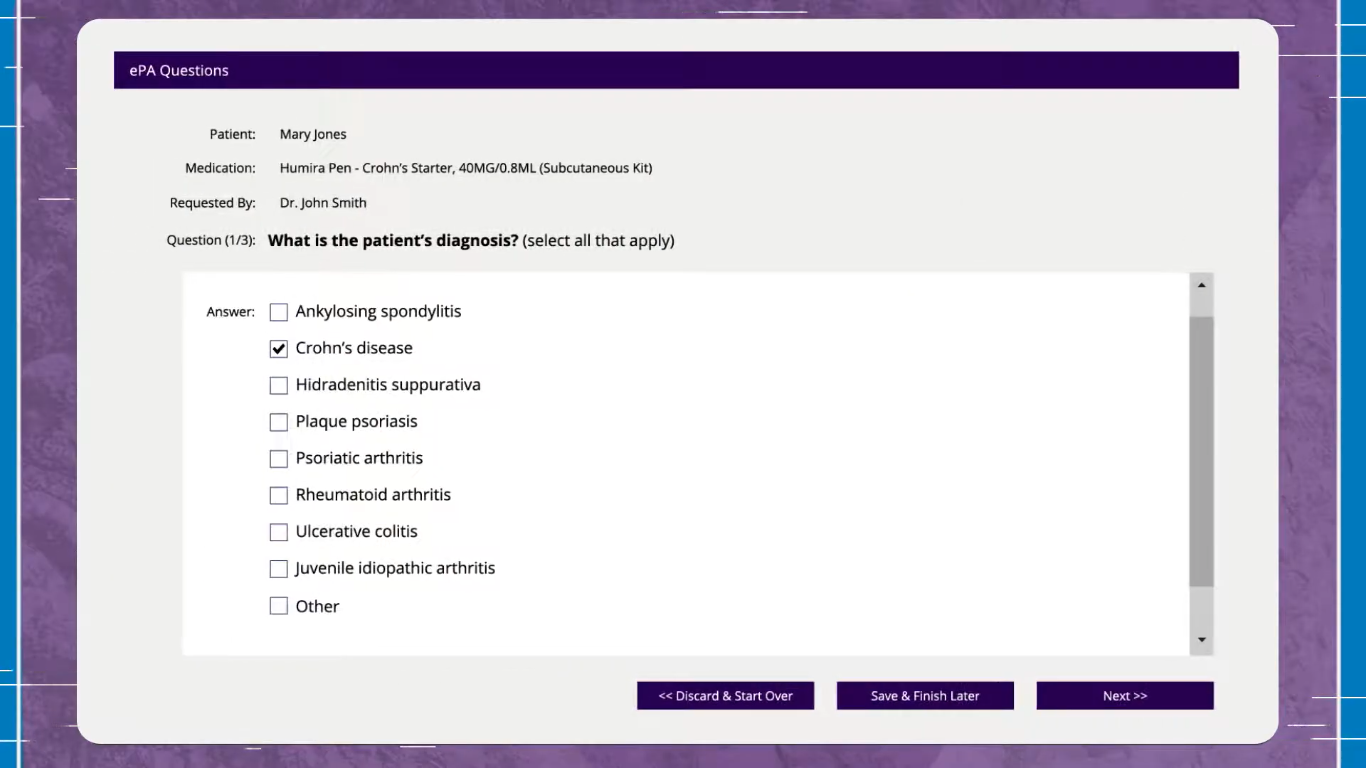
3. Free texts response
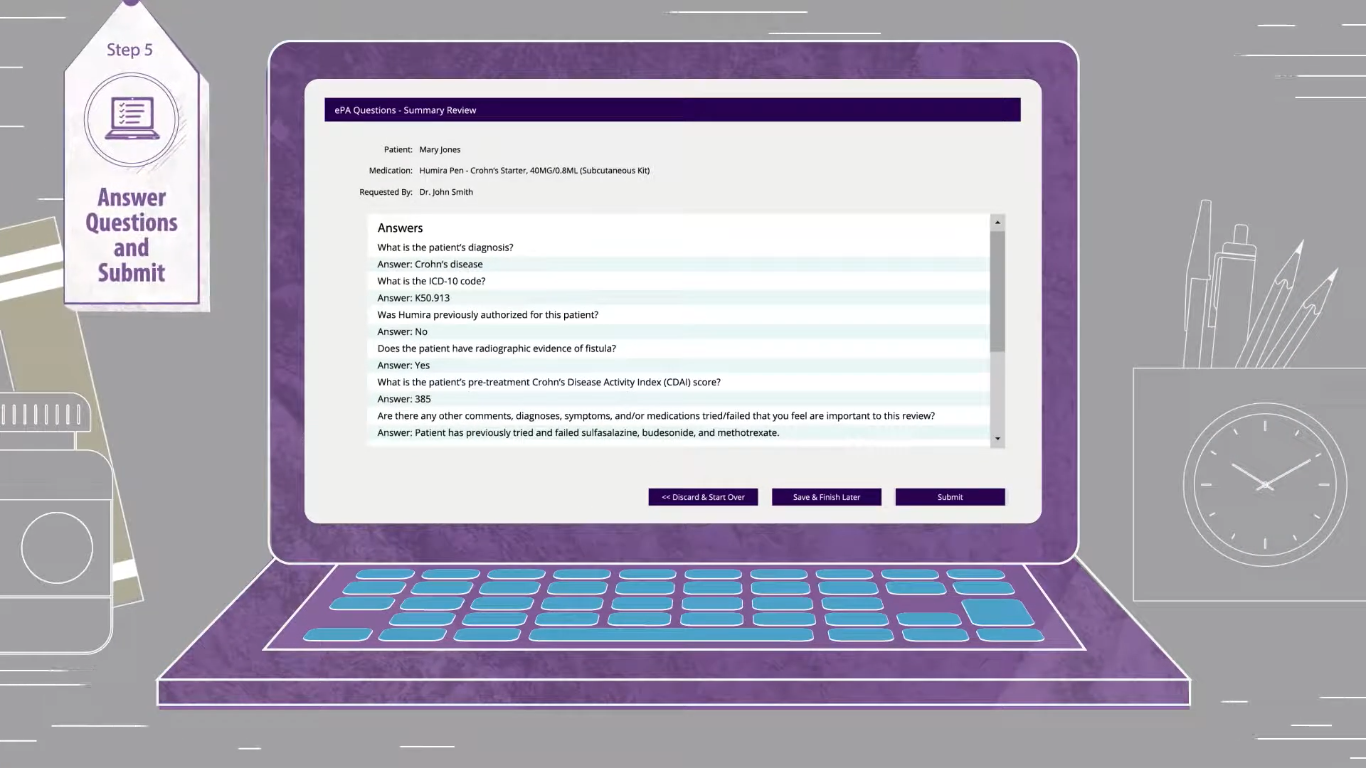
Step 5: Answer questions and submit
This is a crucial step as it may create a conflict between you, the pharmacy, and the payers.
Here, you or other staff members need to validate all the answers you have given regarding the medication plan.
You can explore all answers from a single screen.
Step 6: Now sit, relax, and wait for the confirmation
Once you submit all the answers, the software will automatically –
- Check the eligibility of the medication plan you have chosen
- Patients’ financial responsibilities
It uses AI algorithms and RPA technology to perform these tasks.
And this process sometimes takes less than 2 minutes.
Once it is done, it will send a real-time notification to you.
In case a change is needed, it sends an instant notification to you.
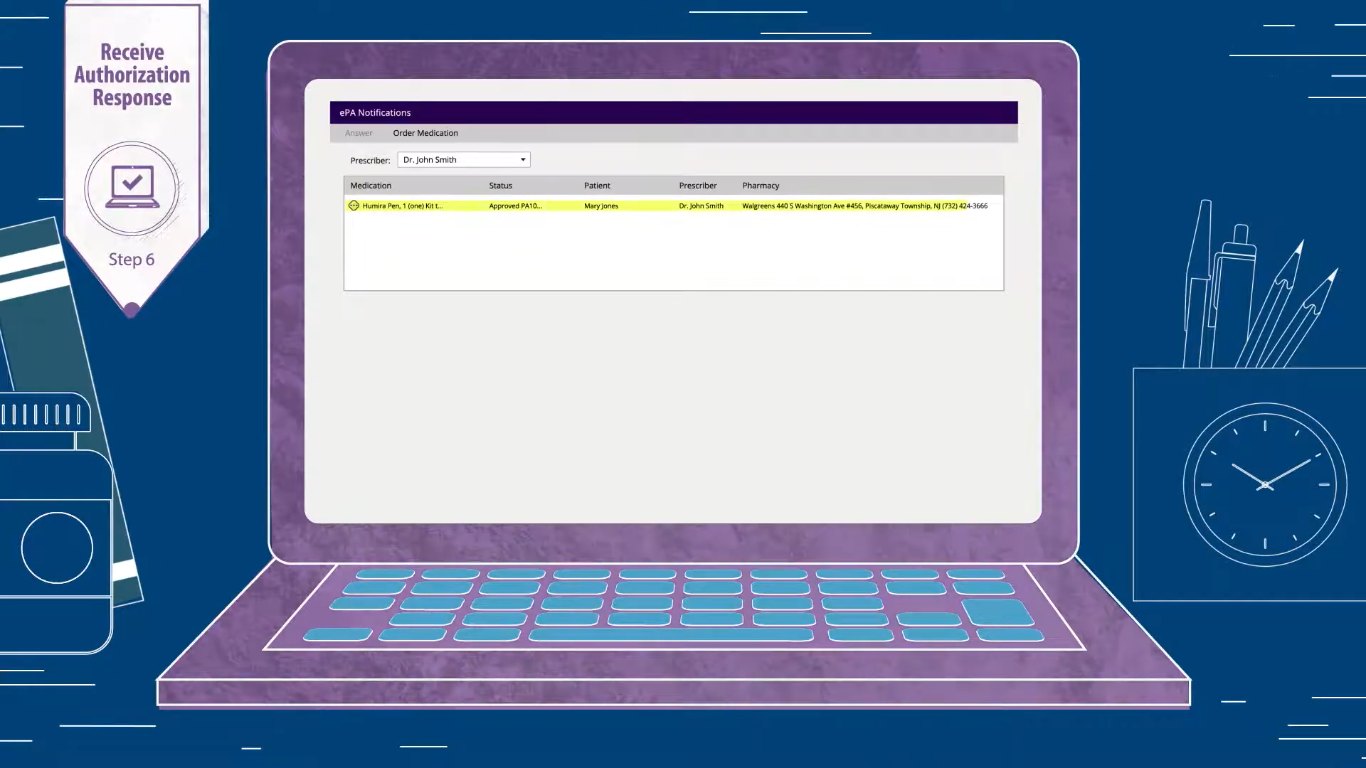
Once a request is approved, you can send an ePrescription note to the pharmacy via SMS and email.
This entire approach ensures that patients won’t face care delays due to the unmet prior authorization processes.
Four Crucial Tasks You Can Automate with Prior Authorization Software
The electronic prior authorization system works on RPA technology.
It helps you automate almost 80% of your workflows including,
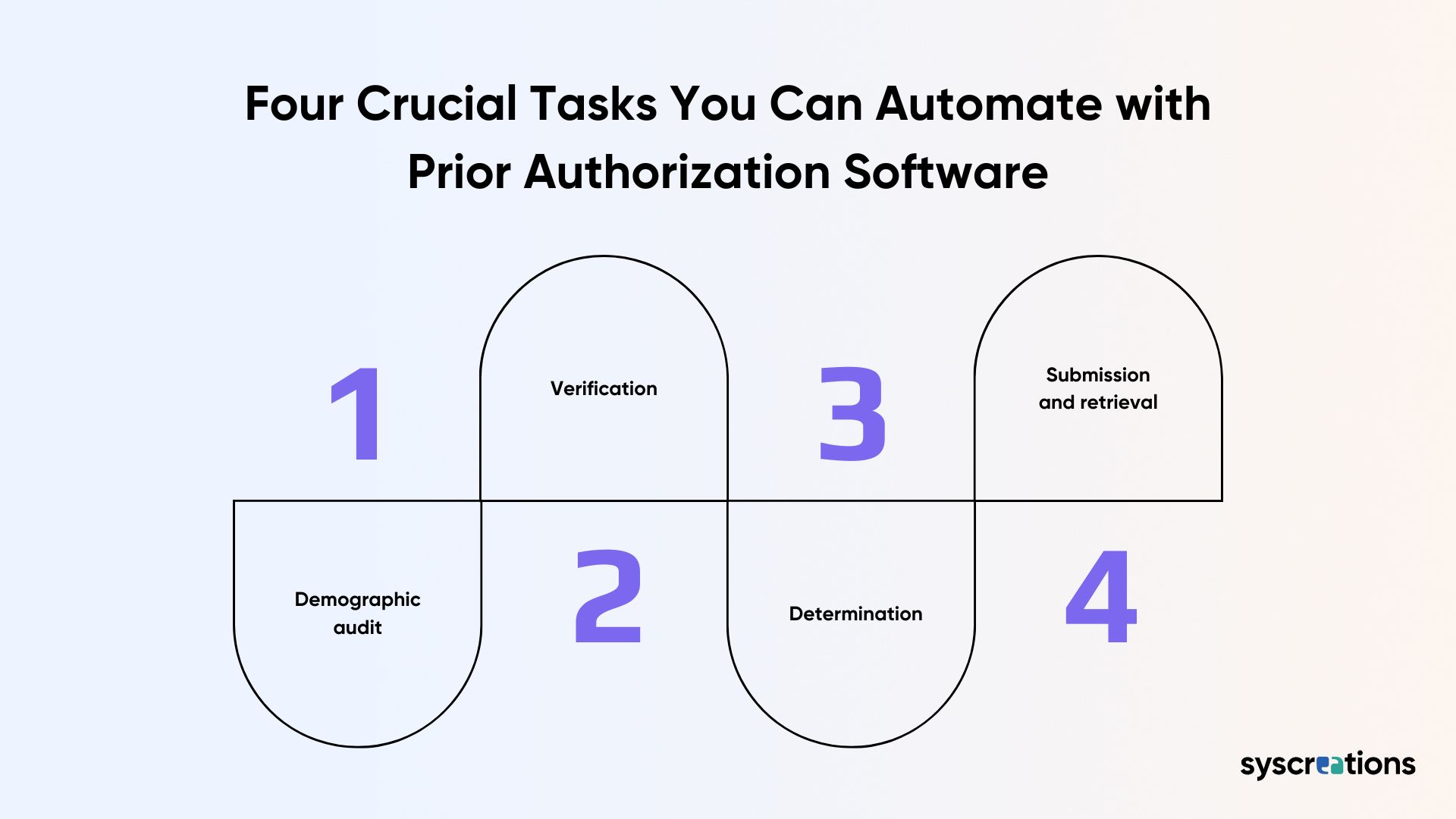
1. Demographic audit
It’s important to eliminate the errors in the patient’s demographic data.
Because it may result in
- Resubmissions
- Denials
- Lost revenue
By using the software, you can automate this entire process.
For example,
- Audit to prevent financial and administrative errors
- Real-time alerts when an error occurs
2. Verification
You can automate two verifications:
- Eligibility
- Medical and prescription benefits
3. Determination
Undeniably, this is the most time-consuming part of prior authorization.
Because providers need to check everything manually to determine whether the authorization is required or not.
But the software totally eliminates the need to check manually.
With just one click, it lets you determine the prior authorization needed.
4. Submission and retrieval
You can also automate the submission process.
For example,
- Automate reminders to payer regarding the submission
- Real-time notification in case of the rework
- Review authorization status without any need for phone calls
- Notification when the prior authorization is confirmed

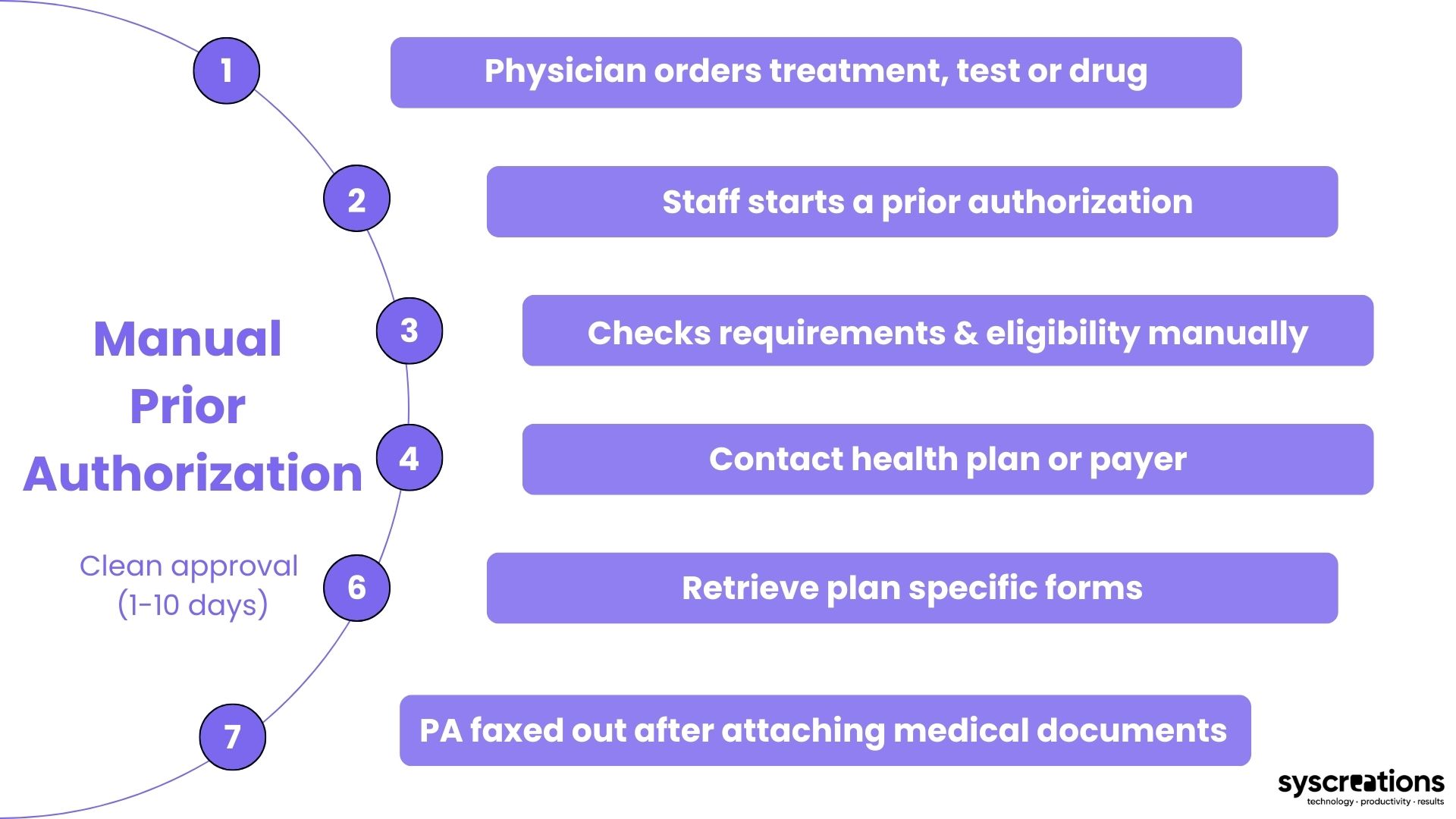
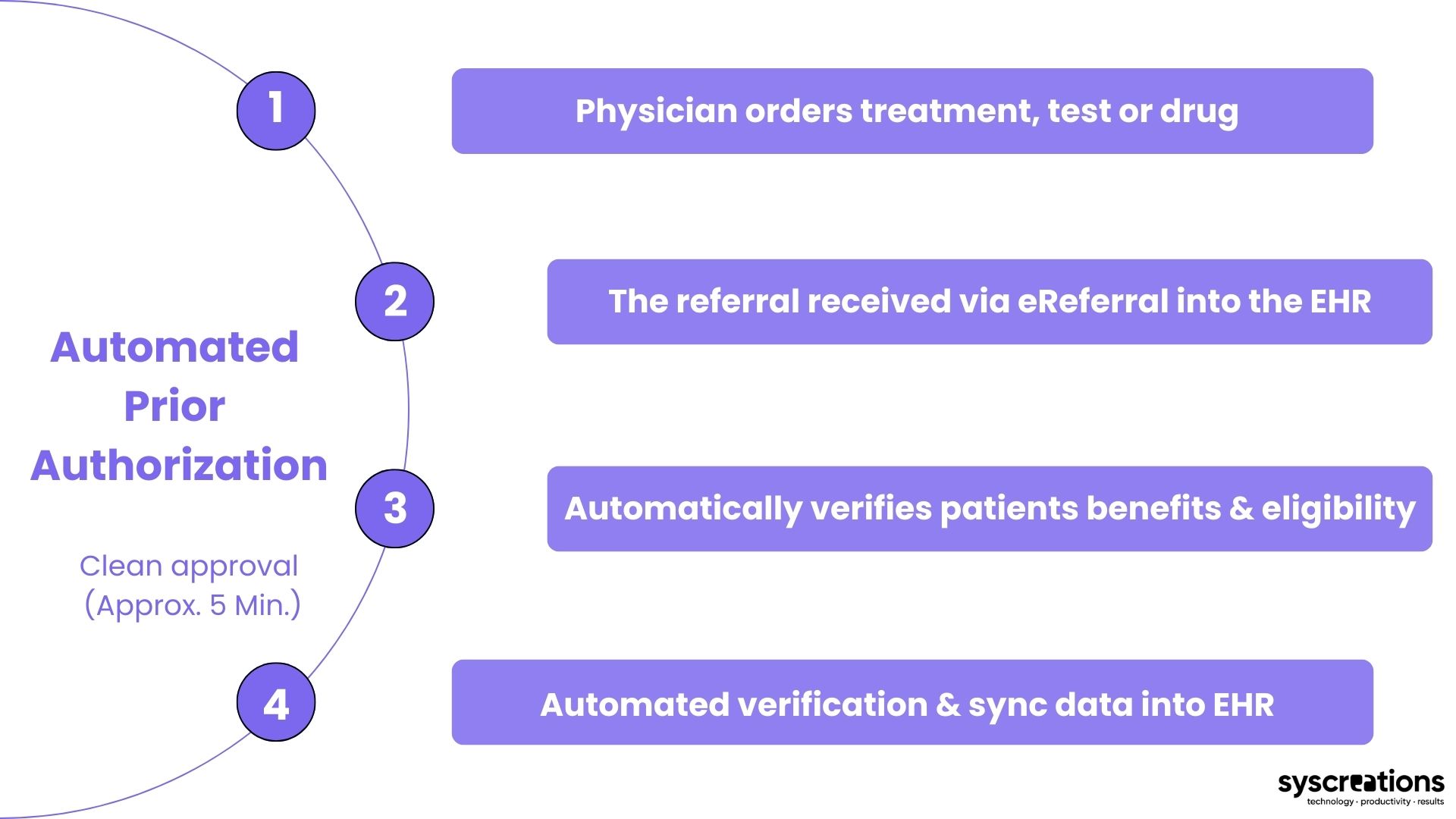
What is the Importance of Having Automated Electronic Prior Authorization?
Let's understand with the simple difference between manual and automated prior authorization approaches.
1. Manual process: You'll get clear approval in 1 to 10 days
2. Automated process: You'll get clear approval in less than 5 minutes
What are the Benefits of an Automated Prior Authorization System?
The electronic prior authorization software brings the patients, providers, and payers under the same roof.
And the following are the top benefits of it.
- No need to fill out the prior authorization form
- No need for Fax and phone calls
- Eliminates the data entry process
- Can avoid performing multiple tasks at the same time
- Completely match your ePrescribing workflows
- Reduces the processing time
- Accelerate patient time to treatment
- Lowers the chances of claim rejection at drug pharmacy
- Reduces administrative burden
- Boost patient satisfaction
Want to Automate your Prior Authorization with Software? We Can Help You with Our 3Es
We are an Ontario-based healthcare IT company.
And we are well-known in the North American health tech market because of our 3Es.
Expertise:
We entertain only healthcare IT projects for – startups, enterprises, organizations, and individuals.
And we are not just limited to the app and software development.
We also have ultimate expertise in – AI, ML, health tech integration, IoT or wearable device integration, VoIP, and automation.
Experience:
We have extensive experience in breaking business, technical and compliance roadblocks.
And we have been doing it for 8+ years!
Experts:
This is something that sets us apart from the rest of the IT companies.
Every team member on our 50+ IT teams is healthcare-specific!
In other words, they have been performing health tech projects since the first day of their professional careers.
It includes – web and app developers, UI/UX designers, business analysts, compliance specialists, AI and ML experts, RPA engineers, and integration experts.
So, if you want to perform prior authorization with less frustration and more productivity, let’s conduct a call and talk about your ultimate goals!