The Connection Between Medication Errors and Electronic Medical Records
1 year ago
In the era of advancing technology, electronic medical records (EMRs) have revolutionized the healthcare industry.
These digital systems have:
- Enhanced patient care
- Streamlined workflows
- Improved data management
However, with the benefits of EMRs also come challenges and potential risks.
One critical issue that deserves attention is the connection between electronic medical records and medication errors.
The Rise of Electronic Medical Records
Electronic medical records have transformed the way healthcare professionals store, access, and manage patient information.
Unlike traditional paper-based records, EMRs offer a digital platform to record and retrieve patient data, including
- Medical history
- Diagnoses
- Medications
- Allergies
- Test results
These systems allow for seamless communication and collaboration among healthcare providers, enabling real-time access to critical patient information.
EMRs can help reduce drug errors but should not be considered an end-all solution.
Healthcare organizations discovered that just installing EMR systems is not sufficient to avoid drug errors and protect patients.
It costs $20 billion to the US healthcare system annually.
Integrating the medication tracker with the EMR may make a difference.
Meaning, the health systems & hospitals should consider integrated medication management initiatives.
It will combine data from multiple devices and systems to offer more comprehensive information to the doctors.
To accomplish this, healthcare leaders will have to ensure that EMRs are used as a part of an integrated medication management system that consists of:
- Pharmacy
- CPOE - Computerized Physician Order Entry
- BCMA - Barcode Medication Administration
- Automated Medication Dispensing
- Inventory Management
- Electronic medication-administration applications
This integration can offer clinicians a comprehensive view of the patient’s drug profile and even help them overcome gaps when different technologies are utilized in isolation.
Understanding Medication Errors
The definition of medication error as per the National Coordinating Council for Medication Error and Prevention (NCCMERP), is:
“… any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is under the health care professionals, patients, or consumer’s control. Such occurrences may be related to professional practice, health care items, procedures, and systems, such as prescribing, order communication, product labeling, packaging, nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use.”
Medication errors occur when there are mistakes or oversights during
- Prescribing medications
- Dispensing medications
- Administering medications
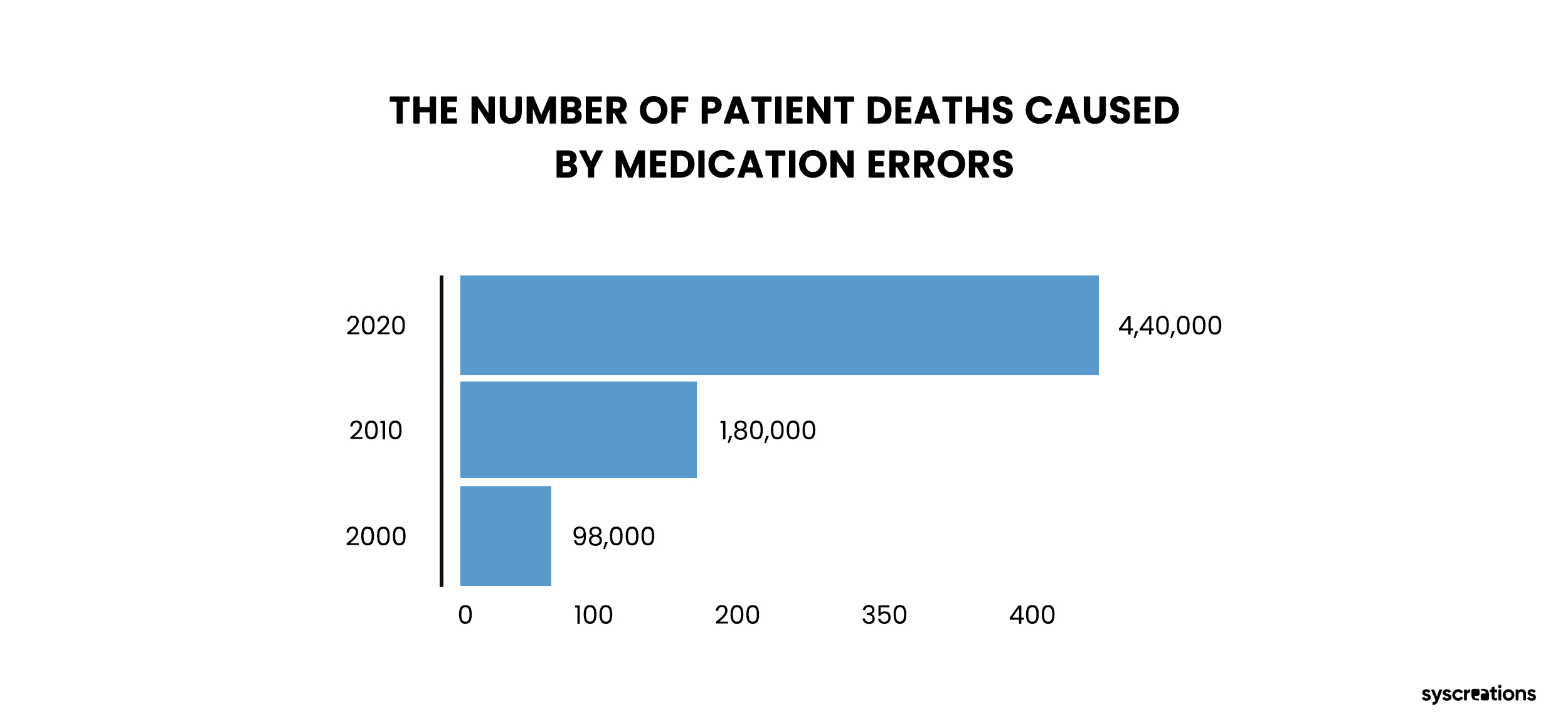
Such errors can have serious consequences, ranging from adverse drug reactions to hospitalizations and even fatalities.
Common Causes of Medication Errors
- Inaccurate diagnosis
- Prescribing errors
- Dose miscalculations
- Poor drug distribution procedures
- Drug and drug device-related difficulties
- Inappropriate drug administration
- Failed communication
- Lack of patient education
The connection between electronic medical records and medication errors lies in how these errors can be inadvertently facilitated or exacerbated by the use of EMRs.
One of the leading causes of therapeutic medication errors is incorrectly administered medication.
The cost of these misadventures to the US economy is more than $177 billion per year.
Potential Causes of Medication Errors in EMRs
1. User Interface Design
Poorly designed user interfaces in EMR systems can lead to confusion and human error.
Cluttered screens, complex navigation, and inadequate medication reconciliation processes can contribute to medication errors.
2. Copy-Paste Functionality
The copy-paste feature, while designed for convenience, can result in inaccurate or outdated information being propagated within a patient's record.
This can lead to incorrect medication orders and potential harm to patients.
3. Alert Fatigue
EMRs often incorporate medication safety alerts to warn healthcare providers of potential issues or conflicts.
However, excessive or poorly tuned alerts can lead to alert fatigue, where clinicians become desensitized to important warnings, increasing the likelihood of medication errors.
4. Lack of Interoperability
Incompatibility or limited interoperability between different EMR systems can hinder the seamless exchange of patient information.
This lack of integration may contribute to incomplete medication histories or missed drug interactions, increasing the risk of medication errors.
Mitigating Medication Errors in EMRs
1. Promoting Patient Safety
EMR-integrated medication management systems can send alerts to patients for preventing drug-to-drug and drug-to-allergy interactions.
It can also control
- Inaccurate dosage
- Duplicate therapy
- Patient status
The connecting link between medication errors and EMR results in better patient outcomes as it assures patient safety.
2. Reduces Drug Diversion and Fraud
EMRs and EHRs can ensure that the prescriptions provided by clinicians are secure and accurate.
EMR integration guarantees the secure and seamless sharing of prescriptions to the pharmacies.
This reduces the chance of medication errors.
3. Prevents Drug Abuse and Misuse
Physicians can access the prescription history of patients in the EMR.
This enables physicians to identify if their patients are involved in drug-abusing behavior.
EMR integration in health systems may enable clinicians to timely intervene in patient’s life and save them.
It can even help in preventing drug abuse.
4. Improves Workflow
With EHRs and EMRs, streamlining the prescription workflows can happen at a centralized location.
It saves time for the clinicians as they won’t have to switch between workflows.
Moreover, this helps doctors to view and prescribe medications without any hassle.
5. Enhances Accuracy
Manual prescribing has loopholes.
Accuracy ceases to be a problem with EMR integration.
It reduces problems leading to medication errors such as
- Illegible handwriting
- Misread abbreviations
- Unclear dosages
Leverage the EMR to Boost Patient Safety and Reduce Medication Errors
To fully leverage the EMR to reduce medication errors and boost patient safety, healthcare providers will have to integrate EMR solutions with additional technologies to become a part of the connected drug management system.
The connection between EMR and medication error can boost the safety and speed of medication management operations.
If you’re looking for a healthcare software development firm to integrate your EMR with other healthcare systems, we’re here to assist you.
We’re a local Canadian healthcare IT company.
With our healthcare-exclusive experience of 8+ years, we’ve helped healthcare organizations in achieving their desired goals within their budget and timeframe.
Fill out the form below and let’s discuss how we can help you achieve your desired healthcare goals.