A Detailed HL7 Integration Guide From HL7 Interface Development Experts

1 year ago
Being in the field of healthcare information technology for more than 7 years and working with more than hundreds of clientele, we are certain about one thing i.e., the two most important and hot topics of the healthcare industry are EHRs and interoperability.
Healthcare providers and hospitals have different systems for executing all the different tasks ranging from billing documents to tracking patients.
They continuously receive and retrieve information from different systems.
But their difference in language, framework, and type of data limit the exchange of information or cause errors.
We know this isn’t Mortal Kombat but fatality will always be open for the patients if the information is not exchanged timely or is full of errors.
Don’t worry!
Have we ever left you hanging?
No.
So, came HL7 integration and loads of questions with it like what is HL7 in healthcare?
Or what is the HL7 interface?
And that is why we have come to you with an HL7 implementation guide!
You must read: Epic skills our HL7 consultants have
What is HL7 in Healthcare? Why Does Healthcare Depend On It?
Health Level- 7 or Health Level Seven International is a nonprofit organization to provide a structure for sharing, exchange, and retrieval of healthcare information electronically.
HL7 standards, widely used across the world, support healthcare delivery as well as the administration, delivery, and evaluation of health services between various healthcare providers.
Acting as a bridge between healthcare and IT giving healthcare providers a smoother way of storing and uniformly moving data.
Being experts in providing healthcare data management services through app and software development, we can assure you with the HL7 implementation guide the need to use different applications and special software for data conversions, handling hard copies, and administrative burden can be reduced while improving the whole care delivery system.
It is done by (HL7 interface development) outlining how data is stored, retrieved, and transported, including the language, data type, and data structure.
These standards are an important step toward interoperability, laying the basis for the development of more open and extensible Fast Healthcare Interoperability Resources (FHIR) and the use of APIs for health IT.
How Does HL7 Integration in Healthcare Work?
Let us tell you a story.
Because, why not?
Stories are always fun, right?
Especially, the ones with happy endings like this one.
There was a patient who visited the ER often and went to see more than one doctor.
But, never carried his entire health record with him.
Every single time he received absolute care without any problem.
What he didn’t know was that the HL7 code was always working in the background just like the internet but it linked health data uniformly.
The standards of HL7 integration helped all his different healthcare providers make better decisions in providing care to him efficiently.
With EHRs in sync, real-time access to his clinical and administrative data without sacrificing his security.
Let us turn our attention toward how HL7 transmits messages.
To understand the process let us accustom you to basic terminologies associated with the HL7 implementation guide.
It consists of a group of segments:
- MSH - Message Header information about a message
- EVN - Event Type event information
- PID - Patient Identification information about a patient
- NK1 - Next of Kin information about the patient's other related parties
- OBR - Observation Request information about an order
- OBX - Observation Report information about a result
The message types are identified by 3 character codes and a trigger event both in conjunction with each other.
HL7’s most commonly used message types-
- QRY- Query, original mode
- BAR – Add/change billing account
- DFT – Detailed financial transaction
- ACK – General acknowledgment
- ADT – Admit, Discharge, Transfer
- RDE – Pharmacy/treatment encoded order
- RGV – Pharmacy/treatment given
- SIU – Scheduling information unsolicited
- MDM – Medical document management
- MFN – Master files notification
- ORM – Order (pharmacy/treatment)
- ORU – Observation result (unsolicited)
And this is an example of how an admission message looks in the HL7:
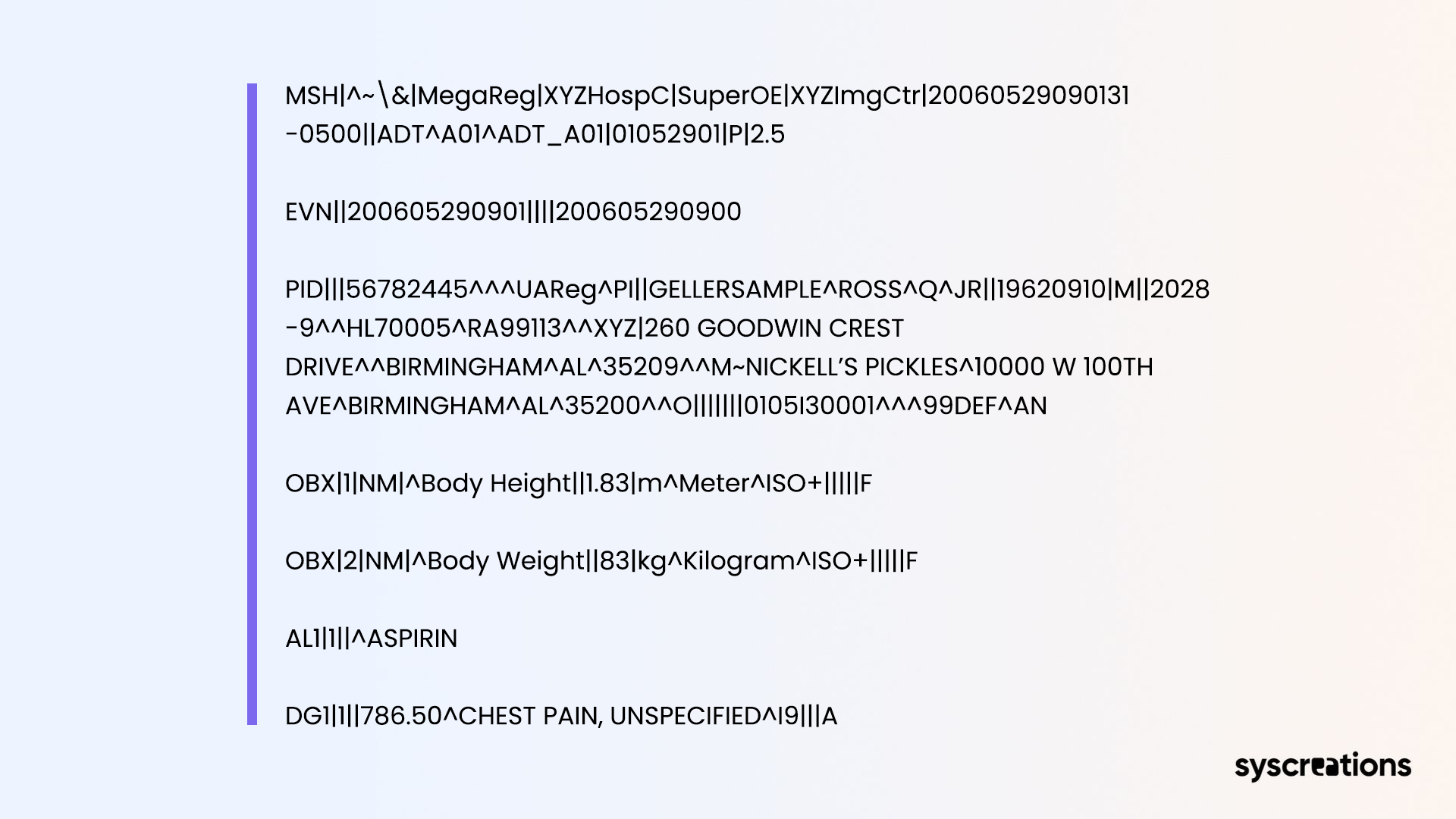
As we told you in the beginning we will be answering all your questions. And the above was the answer for what the HL7 interface is. Moving on…
Take a Close Look at the Categories in the HL7 Implementation Guide that Can Help You Counter Interoperability Issues
The whole implementation guide is divided into major 4 categories defining a new set of rules and standards, building on previous ones as well.
Section 1- Also known as primary standards. These standards are quite essential for interoperability, compliance, and standard system integrations. These are the most popular and widely used standards in these categories.
Section 2- These standards are placed after the implementation of primary standards. It includes links to healthcare providers for messaging and document standards.
Section 3- Describes the use of profiles and models in the construction and management of electronic health records (EHR). Outlines the implementation techniques and offers support papers for other types. This section may also be used as a backup for other standard categories.
Section 4- It includes the implementation rules and recommendations to be used as an aid in programming structure and standards development.
Users are educated and tools are provided to aid in the creation and acceptance of HL7 standards using the Rules and references guide of HL7 interface development.
But what are HL7 standards?
HL7 standards ensure interoperability between healthcare systems even though the systems are part of two different organizations.
EHRs, healthcare providers, healthcare IT vendors, and pharmacies are some of the most common targets that imply HL7 integration into their data exchange structures.
For the above some common standards that are implemented across these healthcare platforms are,
- Continuity of Care Document (CCD) - It promotes interoperability by helping clinicians to facilitate the exchange of electronic medical information to other providers without losing continuity, entitling improvement in patient care.
- Structured Product Labelling - In the HL7 v3, an SPL specification is a document markup standard that describes the structure and syntax of permitted public information that comes with any drug authorized by a medical licensing authority. Targeting biologic drug companies, pharmaceutical companies, and veterinary & bulk drug product companies. It uses sections 1e (version 3), and 2.
- Electronic Messaging Standards - Using the HL7 version 2 product suite, it supports the health industry’s most common interfaces used all over the world. It accomplishes electronic data exchange in the clinical domain with backward compatibility and reduces implementation costs. Targeting exclusively healthcare IT vendors, and providers. It uses Section 1, 1d, and 2.
- Fast Healthcare Interoperability Resources(FHIR) - The most widely used data exchange standard. It enables the exchange of healthcare information among everyone present in the healthcare ecosystem. The exchange can be on mobile apps and cloud communications. Targeting EHRs, healthcare IT vendors, healthcare providers, and pharmaceutical management systems(PMS). It uses Section 1c (all FHIR versions), and 1a (clinical data architecture) CDA.
- Clinical Document Architecture(CDA) - It consists of the discharge summary, admission & physical, pathology report, and imaging report. With a document markup standard, CDA defines the semantics of exchange between a healthcare provider and a patient. Targeting healthcare IT vendors, EHRs & PHR systems, inter-departmental systems, and transcription vendors. It uses Sections 1, 1a, and 2.
We Improved Medication Reconciliation with an HL7 Implementation
It was not long ago when we received an inquiry from a Connecticut-based NGO working with a senior care home. As our team of experts got in touch with them we discovered their problem in delivering medication reconciliation in healthcare.
The issue was to create an improved data-sharing system between them and the healthcare service providers.
Our health IT experts worked together to accelerate the HL7 FHIR standard and delivered a system of value-based care data exchange.
The whole project delivered before the deadline had quite a positive effect.
Successful medication reconciliation was noticed rising from 33% to 42% which was previously 29%.
Information (PHS) from the systems was pulled automatically aiding the staff and reducing the processing time by 7-10 minutes and no reduced hassle for chart monitoring.
These improvements resulted in cost-saving which helped them in investing the rest amount into delivering better care services to the seniors.
We Can Help You with Every Challenge Associated with HL7 and Healthcare Interoperability
Expanding our wings in the healthcare sector, we have been catering to healthcare-specific IT and integration needs.
We have been providing cost-savvy solutions ever since we started.
Unlike other IT companies, we focus on only healthcare and so do the people working with us.
And that’s what makes us very unique.
After all, doing the same and also the specific thing for years is what requires you to be a pro in it.
Let’s have a detailed discussion on your HL7 requirements.
We will guide you through everything and also provide implementation support through our local Canadian healthcare IT experts.